RESUMO
INTRODUÇAO: As queimaduras sao lesoes produzidas por agentes físicos, químicos ou biológicos que podem afetar uma ou várias camadas da pele. A reabilitaçao pediátrica de pacientes queimados cresce dia a dia, devido a muitas razoes: avanços da tecnologia aplicada na pele, aumento da taxa de sobrevida em pacientes queimados, os avanços no projeto de protocolos de reabilitaçao e cooperaçao interdisciplinar para conseguir a recuperaçao máxima possível nestes pacientes.
OBJETIVO: O objetivo deste estudo é demonstrar a eficácia do ultrassom de 3 MHz na reabilitaçao de pacientes queimados com o Scar Scale1 Vancouver, estudos ecográficos de tecidos moles e Escala de Dor Facial -Revisada (FPS-R).
MÉTODO: Os pacientes foram divididos em dois grupos: Grupo A, que receberam a terapia de EUA, de 3 MHz e Grupo B nao receberam terapia.
RESULTADOS: A avaliaçao foi feita por meio da Vancouver Scar Scale (VSS). Uma evoluçao favorável de 75% foi observada no grupo A, ao passo que uma evoluçao desfavorável 8% foi observada no grupo B que nao recebeu terapia de ultrassom de 3 MHz. No relatório de cada ecografia, a média de melhora nos tecidos moles é de 33,6%. A dor diminui a 42,4%. Além disso, no grupo B, a dor aumenta de 15,5%, de acordo com a FPS-R. Esta é a razao pela qual sugere-se que esta terapia melhora a evoluçao de cicatrizes na sua flexibilidade, a altura, a vascularizaçao e a dor.
CONCLUSAO: O uso do ultrassom de 3 MHz é considerado uma terapia alternativa segura e eficaz para pacientes pediátricos com cicatrizes de queimaduras, que estao à procura de reinserçao física, funcional, psicológica e social.
Palavras-chave:
Queimaduras. Ultrassom. Cicratriz. Criança.
ABSTRACT
INTRODUCTION: Burns are lesions produced by physical, chemical or biological agents that can affect one or various layers of the skin. Pediatric rehabilitation of burnt patients grows day by day, due to many reasons: advances of technology applied to the skin, increase of survival rates in burnt patients, advances in the design of protocols in rehabilitation and interdisciplinary cooperation to achieve the maximum possible recovery in these patients.
OBJECTIVE: The objective of this study is to demonstrate the effectiveness of 3 MHz Ultrasound (US) in the rehabilitation of burnt patients with the Vancouver Scar Scale1, echographics studies of soft tissue and Face Pain Scale - Revised (FPS-R).
METHOD: The patients were divided into two groups: Group A that received therapy of US of 3 MHz and Group B did not receive therapy.
RESULTS: Evaluation was done using the Vancouver Scare Scale (VSS). A 75% favorable evolution was observed in the group A, while an 8% unfavorable evolution was observed in the group B that did not receive US therapy of 3 MHz. In the report from each echography, the average of improvement in soft tissues is 33.6%. The pain decreases a 42.4% furthermore in group B the pain increases a 15.5%, according to Face Pain Scale- Revised (FPS-R). This is the reason it is suggested that this therapy improves the evolution of scars in their pliability, height, vascularity and the pain.
CONCLUSION: The use of the 3 MHz ultrasound is considered an effective and safe alternative therapy for pediatric patients with burn scars, who are looking for physical, functional, psychological and social reinsertion.
Keywords:
Ultrasonics. Burns. Scars. Child.
Burns are lesions produced by physical, chemical or biological agents that can affect one or various skin layers. Depending on the depth and extension reached, these lesions leave sequels that hinder the patient's physical, mental and social development
1. The World Health Organization raises the fact that burns cause more than 20 000 deaths a year and in 21 countries holds first place as the major cause of deaths in children between 1 and 4 years-old. They are produced by carelessness or ignorance of potential dangers in certain situations. Infants and young child should receive protection from the environment that surrounds them due to their curiosity as well as their wish to imitate adults
2.
Rehabilitation of pediatrics burn patients is a growing specialty due to various factors: technological development applied to the skin, increased survival rates of burnt patients, progress in the design of rehabilitation protocols and interdisciplinary cooperation to achieve the maximum possible recovery in these patients
3,4.
The normal scarring process involves three phases: inflammatory, proliferative and remodeling. For clinical use, Rohrich and Robinson divided the scarring process into: normal, pathological and unaesthetic. The normal scarring leaves a scar that is aesthetically acceptable and functional. Pathological scarring is subdivided into excessive and insufficient. In the excessive scarring there is an overproduction of scar tissue (keloids, hypertrophic contractures). In insufficient pathological scarring there is a deficit in cicatrization (chronic and unstable wounds). In unaesthetic scarring there takes places a normal process of scarring, but due to its location and direction, cosmetic results are not produced and treatment will be required to improve it
5.
The vast majority of recent therapeutic ultrasound literature centers the fact that therapeutic ultrasound has a frequency range of 0.75-3 MHz, with most machines set at a frequency of 1 or 3 MHz's. Low‐frequency ultrasound waves have greater depth of penetration but are less focused. Ultrasound at a frequency of 1 MHz is absorbed primarily by tissues at a depth of 3-5 cm and is therefore recommended for deeper injuries and in patients with more subcutaneous fat. A frequency of 3 MHz is recommended for more superficial lesions at depths of 1-2 cm
6,7. Ultrasound may induce thermal and non‐thermal physical effects on tissues. Non‐thermal effects can be achieved with or without thermal effects. Thermal effects of ultrasound upon tissue may include increased blood flow, reduction in muscle spasm, increased extensibility of collagen fibers and a pro‐inflammatory response
8.
The objective of this study is to demonstrate the effectiveness of 3 MHz Ultrasound in the rehabilitation of burnt patients with the Vancouver Scar Scale
9, echographics studies of soft tissue that show the decrease of scar thickness and Face Pain Scale - Revised (FPS-R)
10.
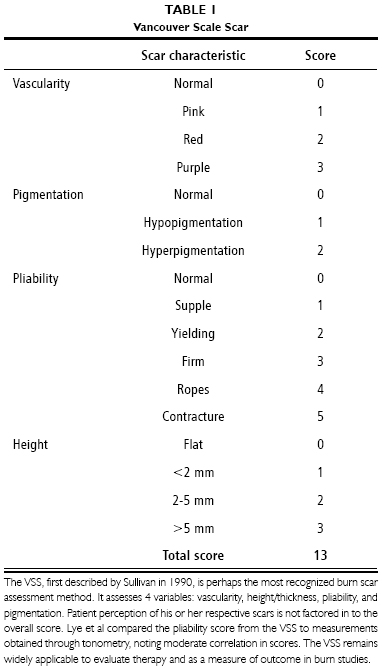
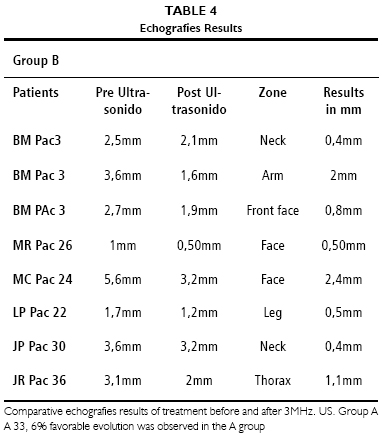
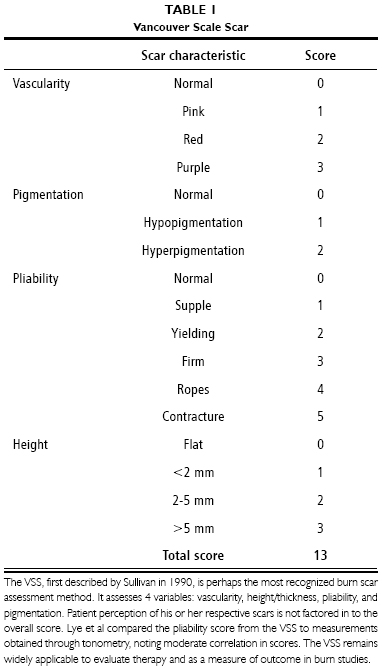
METHOD An experimental and descriptive, study was performed on a total of 45 patients, 19 females and 26 males, ranging from an age of 2 to 14 at Children's Hospital Cordoba, Argentina. The patients presented a diagnosis of hypertrophic scarring caused by second and third degrees burns in different parts of the body. Data on age, sex, burning elements, type of burn, surface area, social and economical levels were collected through the revision of medical records and kinesiology charts. Semiological valuation was also recorded with the Vancouver Scare Scale (VSS) (Table 1), which included pliability, height, vascularity and pigmentation.
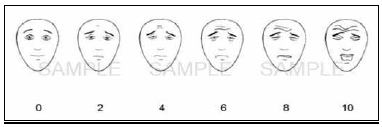
The second method of evaluation consisted on the examination of echographies performed on soft tissues on patients from the beginning to the end of treatment. The third method of evaluation was the Faces Pain Scale - Revised (FPS-R) (Figure 1) is a self-report measure of pain intensity developed for children. It was adapted from the Faces Pain Scale in order to make it possible to score on the widely accepted 0-to-10 metric.
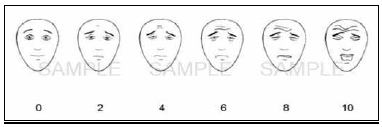
Figure 1 - Faces Pain Scale - Revised,
c2001, International Association for the Study of Pain For clinical, educational, or research purposes, use of the FPS-R
Patients were divided into two groups, Group A, 36 patients receiving a 3 minute treatment in 10 x 10 cm. areas twice a week with 3MHz ultrasound (1,9 w/cm2) during 3 to 8 month period (Table 2). And the group B with 9 patients who did not receive treatment, due to different motives: distances from where they receive treatment, lack of economic means to travel to the institution were therapy is free, lack for responsibility for the tutors, etc. (Table 3). The scarring evolution was observed on both groups on patients that had received 3 MHz U.S. treatment as well as those that have not received the therapy.
RESULTS
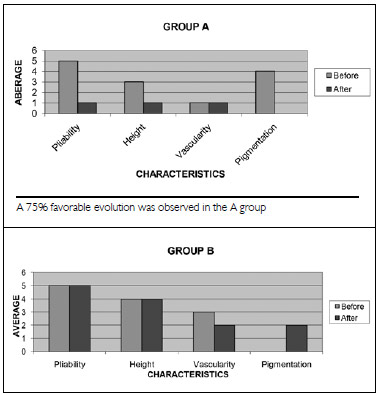
Vancouver Scar Scale All values in group A decreased: the pliability had evolved from 5 to 1, height from 3 to 0, vascularity from 3 to 1, and pigmentation was maintained at 1 without evolution. In group B it was recorded, averaging each value, that pliability remained without evolution at 5, the same as height at 4, vascularity evolved from 3 to 2, while the pigmentation of 0 to 4 (Figure 2).
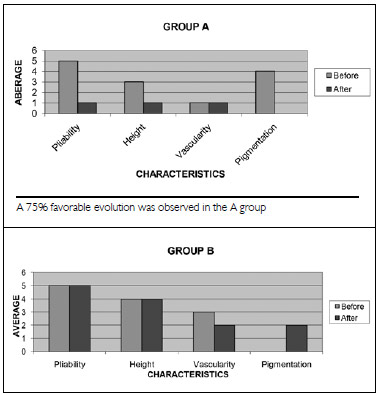
Figure 2 - An 8% unfavorable evolution was observed in the B group that did not received U.S. therapy of 3 MHz.
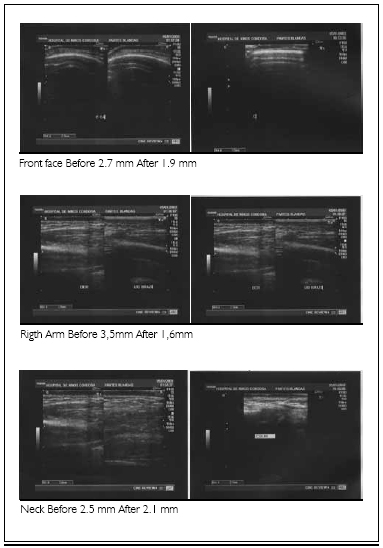
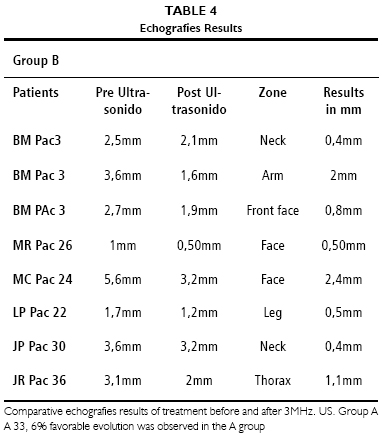
Eight pairs of echographies of scare tissues were analyzed, before and after treatment with 3 MHz Ultrasound, where evolutions of scars of 6 patients from group A were observed (Figures 3 to 8). In the report from each echography, it is recorded a decrease from 0.5 mm to 2.4 mm in soft tissues parts where 3 MHz Ultrasound therapy was applied (Table 4).
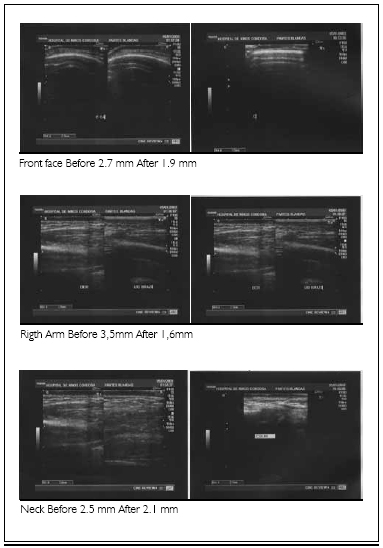
Figure 3 - Group A - patient 3
Figure 4 - Group A - patient 26 - Face Before 1 mm After 0.5 mm
Figure 5 - Group A - patient 22 - Leg Before 1.7 mm After 1.2 mm
Figure 6 - Group A - patient 24 - Face Before 5.6 mm After 3.2 mm
Figure 7 - Group A - patient 30 - Neck Before 3.6 mm After 3.2 mm
Figure 8 - Group A - patient 36 - Thorax Before 3.1 mm After 2 mm
Face Pain Scale - Revised (FPS-R)
It was observed that all values in group A, the pain had decreased from 8 to 3. Furthermore, in group B the pain increases from 8 to 9.5 (Table 5).
DISCUSSION Scars presented a 75% favorable evolution with the use of 3MHz ultrasound. An 8% unfavorable evolution was observed in the group B that did not received US therapy of 3 MHz. In both cases results were averaged considering all the characteristics in equal values. The average of improvement in soft tissues is of 33.6% (echography). The pain decreases a 42.4% in group A, furthermore in group B the pain increases a 15.5%. It has been reordered in many investigations that "micro-massage" produced by ultrasonic waves (related or not to thermical effects) may be another useful method to improve the scarring tissue quality
11. However no significant national and international facts have been found, thus not generating sufficient data to revise.
CONCLUSION The groups under study have contributed proof to the effectiveness of the 3 MHz Ultrasound in the treatment of pediatric patients with burn scars. The differences in results between groups are statistically significant, which lets us recommend the inclusion of treatment with 3 MHz Ultrasound in patients with burn scars. Said treatment improves evolution of pliability, height, vascularity, pain and decreases the thickness of the scar. It is considered that the 3 MHz ultrasound is an effective and safe therapeutic alternative for pediatric patients with burn scars, who are hoping for improvement of skin quality.
REFERENCES 1. Herndon DN. Tratamiento integral de las quemaduras. Barcelona: Elsevier Masson; 2009 . p.343-53, 421-50.
2. WHO - World Health Organization - Bulletim. [Acessed June 22, 2013].Available from:
www.who.int/bulletin/volumes/87/5/08-059535-ab/es/ 3. Blanco MGR. Abordaje Integral en la rehabilitación de pacientes quemados pediátricos. In: XIV Congreso Argentino de Quemaduras; 2011; Mar del Plata. Anais. Mar del Plata. p.34.
4. Blanco MGR. Abordaje Integral en la rehabilitación de pacientes quemados pediátricos con quemaduras tipo B en el 86% de la superficie corporal total. In: XIV Congreso Argentino de Quemaduras; 2011; Mar del Plata. Anais. Mar del Plata.. p.33.
5. Ezpinosa AFR, Enríquez JM, alcalá DP, Peralta MLP. Efectividad de la bleomicina intralesional para el tratamiento de pacientes con cicatrices queloide. Estudio comparativo con dexametasona. Dermatologia Rev Mex. 2011;55(3):119-26.
6. Gann N. Ultrasound: current concepts. Clin Manage.1991;11:64-9.
7. Ziskin M, McDiarmid T, Michlovitz S. Therapeutic ultrasound. In: Michlovitz S, ed. Thermal agents in rehabilitation. Philadelphia: FA Davis; 1990.
8. Dyson M. Mechanisms involved in therapeutic ultrasound. Physiotherapy. 1987;73(3):116-20.
9. Cheng W, Saing H, Zhou H, Han Y, Peh W, Tam PK. Ultrasound assessment of scald scars in Asian Children receiving pressure garment therapy. J Pediatr Surg. 2001;36(3):466-9.
10. Hicks CL, von Baeyer CL, Spafford P, van Korlaar I, Goodenough B. The Faces Pain Scale-Revised: toward a common metric in pediatric pain measurement. Pain, 2001;93(2):173-83.
11. Rocha R. La fisioterapia y las cicatrices hipertróficas: el poder de las fuerzas mecânicas. [Acessed 2013 June 23]. Available from:
http:www.efisioterapia.net/articulos/imprimir.php?id=350&p=350-efisioterapia.pdf 03/09/
1. Physical Therapist of the Children Hospital, Area of Rehabilitation of Plastic Surgery. Professor at the National University of Cordoba College of Kinesiology
2. Physical Therapist
Correspondência:
María Gabriela Ruiz Blanco
G. Sayago 2337 Fuencarral PB D B° Parque Vélez Sarsfield 5016
Córdoba, Argentina
E-mail:
lagabiruiz@hotmail.com Artigo recebido: 11/2/2013
Artigo aceito: 21/4/2013
Trabalho realizado no Hospital Infantil, Córdoba, Argentina.